Dr. Alessio Bernasconi, MD, FEBOT and his colleagues at the Royal National Orthopaedic Hospital in London have produced critical and salient findings about the role of weight-bearing CT imaging (WBCT) in assessing pes cavovarus.
Dr. Bernasconi recently shared these findings in a FOOTinnovate webinar, and his presentation is outlined below.
Click here to watch the FOOTInnovate webinar. A FOOTInnovate account is required.
A Refresher on Pes Cavovarus Diagnosing Procedures
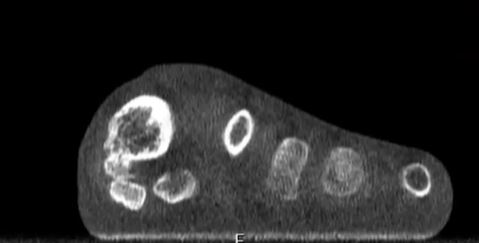
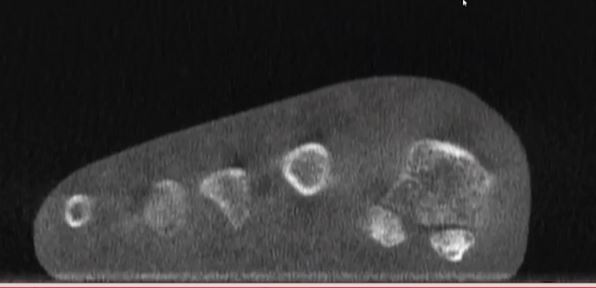
Pes cavovarus is considered a three-dimensional deformity and is characterized by a high-arched, varus hindfoot alignment with a forefoot that may be abducted or plantarflexed depending on the individual case.
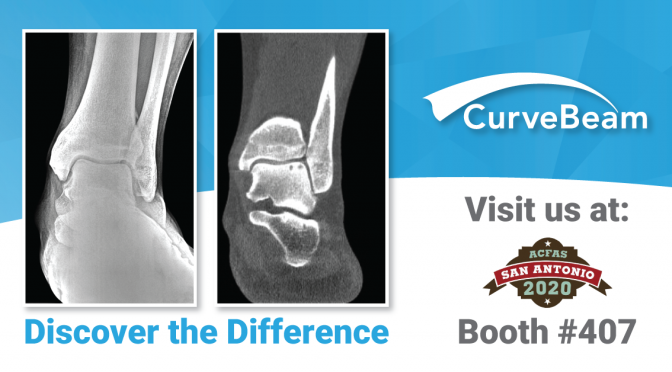
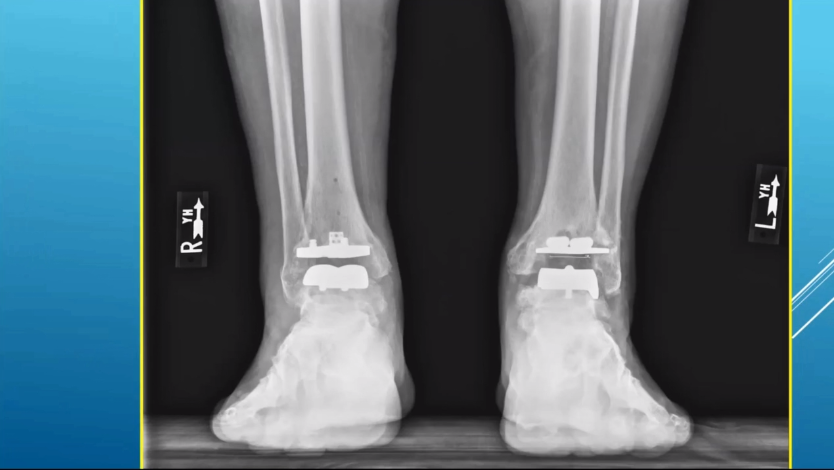
Diagnostic work for pes cavovarus is based on a thorough clinical assessment. However, additional imaging is needed, and X-Ray imaging is the current standard. Additional CT or MRI imaging can be ordered to further characterize the deformity and assess the status of joints and soft tissues.
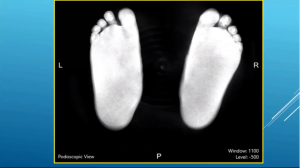
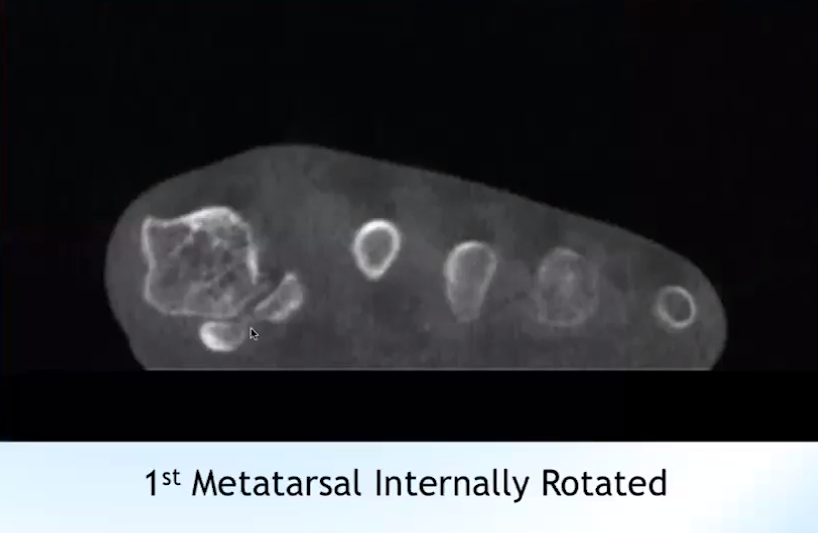
However, common dorsoplantar, lateral views of bilateral cavovarus deformity can bring along with them difficulty in precisely identifying joint planes and status. Recent studies, including published papers from PubMed suggest that radiographs have inherent bias as beam position, operators, foot position, and more can change what doctors see and identify.
Is there any objective way to identify hindfoot alignment?
Improving Identification of Hindfoot Alignment
The Saltzman view – developed by Charles Saltzman, MD and Georges El-Khoury, MD – is designed to find the main axis of the tibia and the main axis of the calcaneus, then to define the angle between those two lines.
However, this view can still be limited by rotation of the foot.
That’s why authors like Jonathan Kaplan, MD, who outlined a solution in Foot & Ankle International, propose the use of weight-bearing CT scanning as a better alternative when diagnosing malalignment associated with pes cavovarus.
The Implications of Weight-Bearing CT Scanning
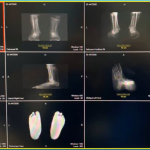
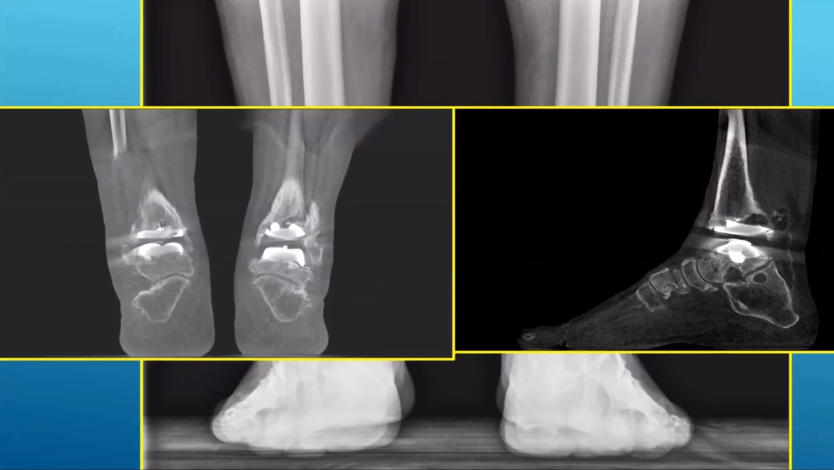
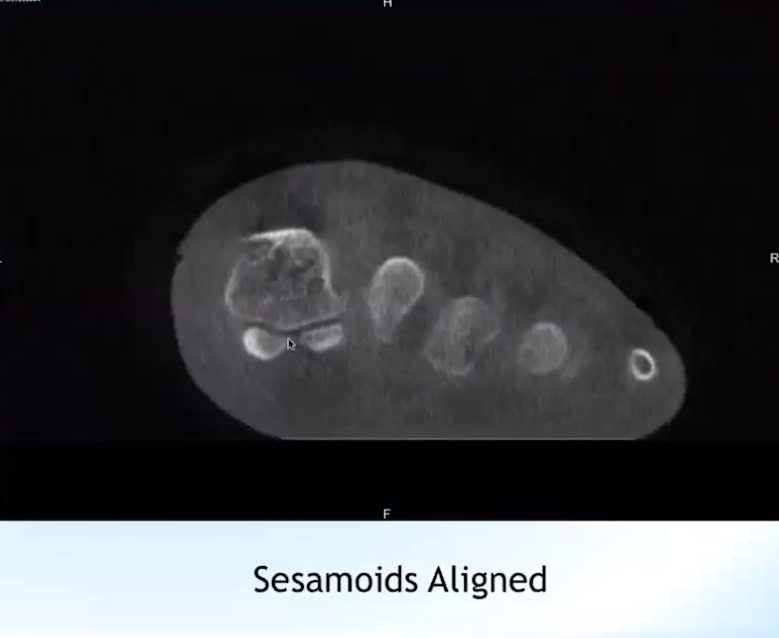
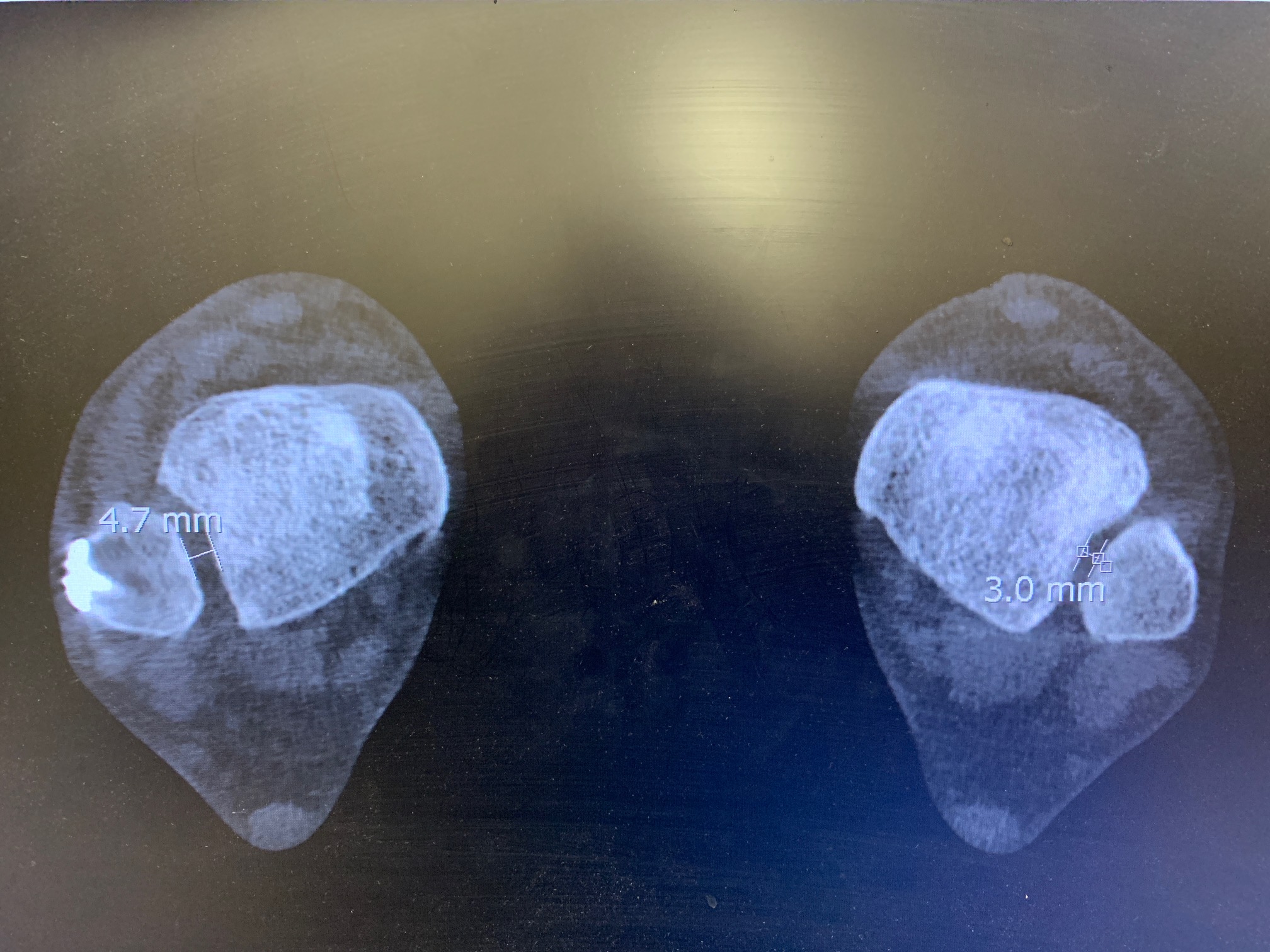
Two studies published in 2017 and 2018 introduced the idea of using three-dimensional measurements on weight-bearing CT images, allowing the measurement of malalignment to move away from a single plane and toward a volume-based view that produces a more reliable and true view of the bones in physical space.
The three measurements proposed are foot and ankle offsets, the calcaneal offset and the hindfoot alignment angle.
In 2017, a study assessing 135 datasets including normally aligned feet, varus hindfeet and valgus hindfeet demonstrated excellent inter and intra-observer reliability using this new measurement.
The true revolution in utilizing 3D measurements is that, in gathering the three measurements, you can add a fourth point to represent volume that provides that additional beneficial depth.
“What you need is a cone-beam, weight-bearing CT device,” Dr. Bernasconi said. “In our institution, we use the PedCAT one. You need a software to elaborate data – CubeVue – and you need a TALAS plug-in.”
Essentially, Dr. Bernasconi said, this landmark software solution can provide a simpler way to obtain values relative to the normative values that highlight varus or valgus malalignment.
Critical Questions
Dr. Bernasconi highlighted three critical questions regarding the reliability of this new solution:
- How reliable are 3D measurements when diagnosing pes cavovarus?
- Does etiology affect reliability?
- Does the severity of the deformity affect reliability?
To find the answers, Dr. Bernasconi and the staff at the Royal National Orthopaedic Hospital completed a retrospective study based on STROBE guidelines of patients with a pes cavovarus diagnosis from their hospital between 2015 and 2017.
Eventually settling on 17 patients, the team matched those patients with an equal number of normally aligned feet. Three observers with different levels of expertise and different knowledge of the weight-bearing CT imaging process produced excellent inter-observer reliability. Further, there was little variance between the observers, suggesting that the data is reliable regardless of previous expertise, etiology and deformity severity.
“The reason that we have studied foot morphology, thanks to the help, obviously, of this new technology, (is that) standing CT allows you to reproduce in a more faithful way the true geometry of the bone and the joints in the space,” Dr. Bernasconi said. “We think that this may potentially help us better understand the etiology.”
Though Dr. Bernasconi said his findings were far from enough to fully corroborate this positive outcome, they are certainly a starting point.
The takeaway, he said, is that this new, 3D approach will allow for reliable assessment of pes cavovarus, both in the diagnosing stage and in monitoring patients after procedures to determine how successful the correction was.