Dr. Matthew Welck presented findings from a study overseen by Dr. Mark Myerson at the British Orthopedic Foot & Ankle Society (BOFAS) meeting in Bristol, England, in early November.
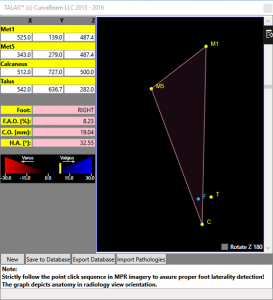
The study compared three hindfoot alignment measurements: radiographic hindfoot moment arm, radiographic hindfoot alignment angle, and TALAS. TALAS is a semi-automatic measurement based on anatomical landmarks on a weight bearing CT scan. TALAS was found to have the best intra-observer reliability.
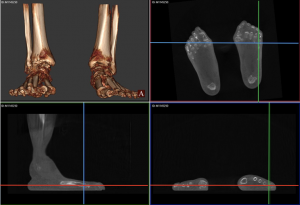
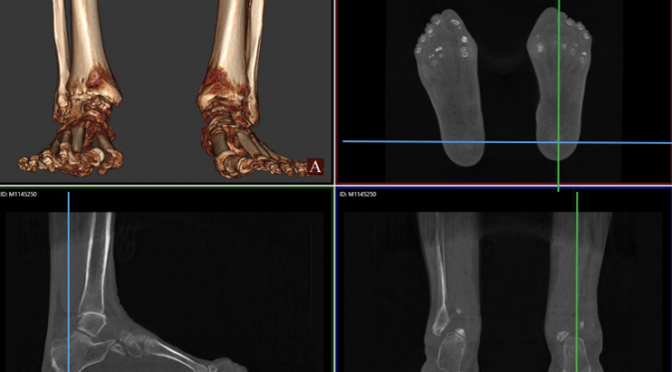
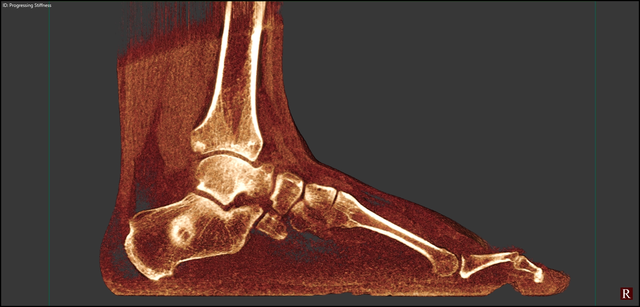
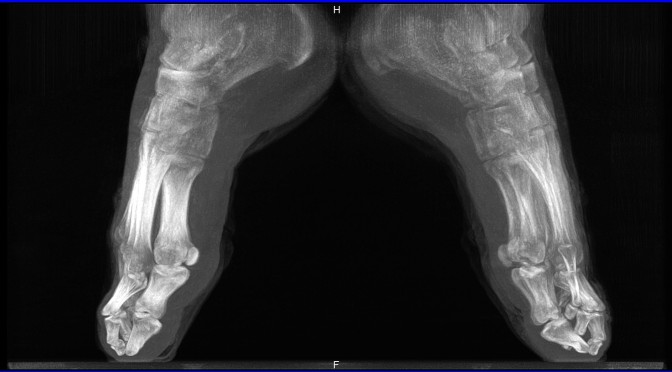
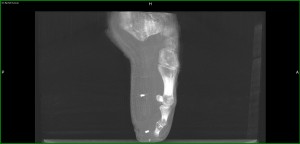
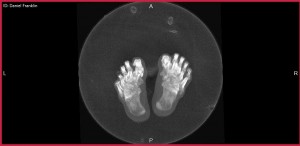
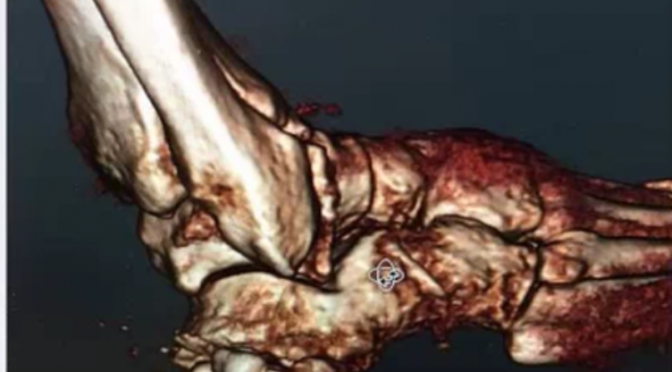
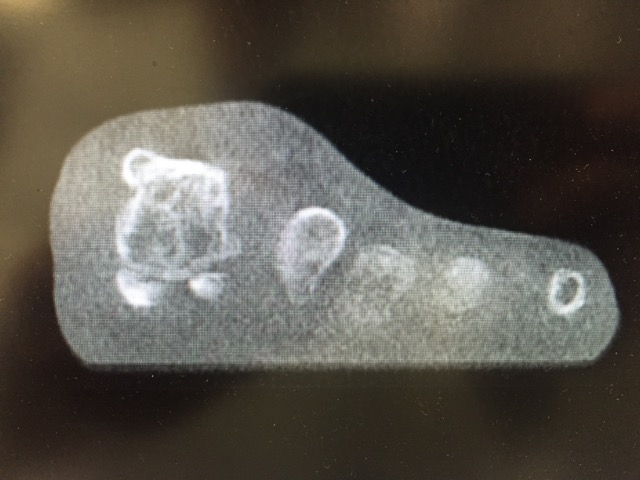
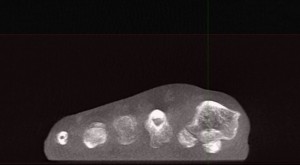
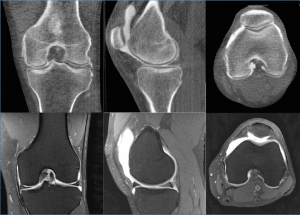
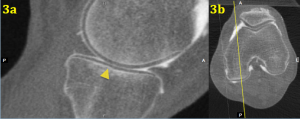
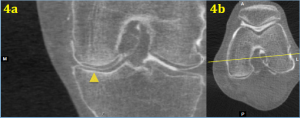
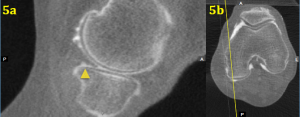
As Dr. Welck explained, the TALAS technique measures offset of midline of whole foot, rather than just calcaneus. He presented an example of a patient with ‘neutral’ alignment to compare hindfoot alignment measurements. The first point was placed on the superior weight bearing portion of the talar dome. The calcaneus contact point was then placed on the lowest point of the calcaneus. The first metatarsal contact point was placed on the lowest point of the first metatarsal head. Similarly, the 5th metatarsal contact point was placed on the lowest point of the 5th metatarsal head. TALAS software provided a mapping of these contact points showing the axis, or the ’true’ hindfoot alignment.Next, Dr. Welck summarized the intra and inter observer reliability among the three measurements. As previously shown in the literature, Dr. Welck explained, there is good intraobserver reliability with the Saltzman hindfoot moment arm technique. Similarly, the hindfoot alignment angle has excellent intraobserver reliability. And there was excellent intra-observer reliability among investigators. Dr. Welck noted that while all three measurement techniques are reliable, the CT Ground Reactive Force Technique was nearly perfect.
CurveBeam’s pedCAT provides bilateral, weight bearing 3D CT imaging of the foot and ankle, greatly surpassing traditional imaging methods such as X-Ray and CT studies. CurveBeam’s technology also reduces the number of patient trips to the hospital, and exposes patients to less radiation. Because the 3D data generated by pedCAT is far more robust than could be interpreted by available software, CurveBeam engineers are collaborating with leading foot and ankle surgeons to develop a new measurement software – TALAS. TALAS, or Torque Ankle Lever Arm System, is a feature within pedCAT’s visualization application CubeVue.
The British Orthopaedic Foot & Ankle Society (BOFAS) is a society of orthopaedic surgeons who have a special interest in surgery of the foot and ankle. The Society works to encourage interest in foot and ankle surgery among orthopaedic surgeons and to encourage both basic science and clinical research in the field.