As the orthopaedic and podiatric specialties continue to advance, there is great potential for technology like CurveBeam’s pedCAT system to revolutionize care.
Recent research highlighted the importance of weight bearing scans to the understanding of foot and ankle anatomy, suggesting a role for pedCAT in both a research and clinical setting. “Rotational Dynamics of the Normal Distal Tibiofibular Joint with Weight-Bearing.
Computed Tomography” a 2016 study published in Volume 37 of
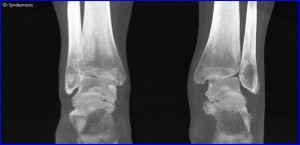 Foot & Ankle International sought to determine the normal range of motion for uninjured distal tibiofibular joints. Researchers hoped this reference would be useful as a comparison when assessing injured and repaired ankles.
Foot & Ankle International sought to determine the normal range of motion for uninjured distal tibiofibular joints. Researchers hoped this reference would be useful as a comparison when assessing injured and repaired ankles.
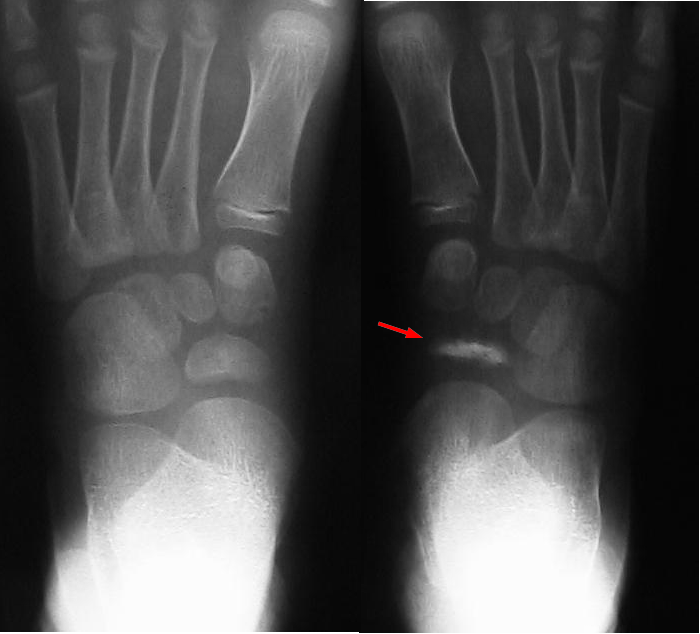
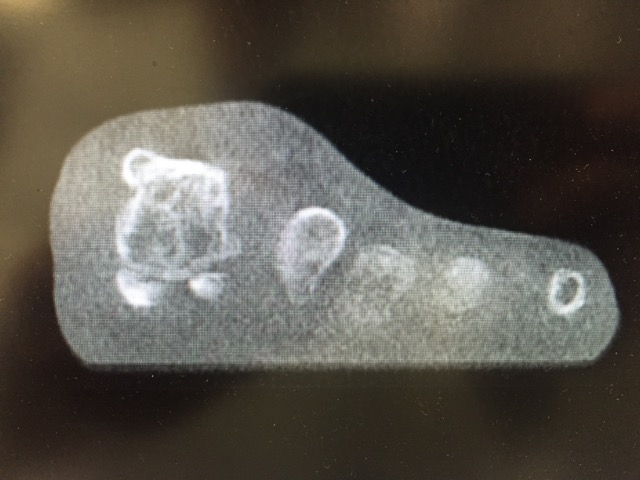
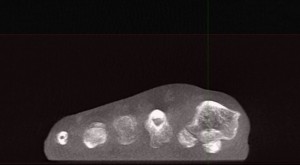
Until recently, all measurements of this motion had been conducted on cadavers or through non-weight bearing scans. In contrast, this study used a weight-bearing CT (WBCT) system to survey the ankles of 32 subjects as they stood on one foot, then the other.
They found a “total movement of 1.5 mm and rotation of 3 degrees” in the syndesmosis as the average across subjects. However, the study also found that intersubject variation was extremely high, meaning different people had vastly different ranges of motion despite similar orthopaedic histories.
These differences were not correlated with sex or age. Intrasubject variation, or the difference in movement between a person’s right and left foot, was significantly smaller and more consistent, less than 1 mm on average.
The study therefore concluded “the contralateral ankle should be used as a reference when dynamic alignment of the distal tibiofibular joint is studied.”
In other words, surveying a person’s uninjured ankle will give a better idea of what is normal movement for that particular individual than comparing the injured ankle to a standardized range, like the one this study endeavored to produce.
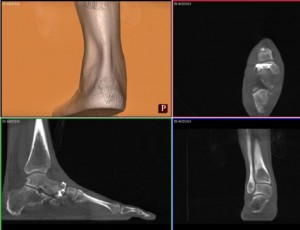
CurveBeam’s pedCAT technology could have helped researchers eliminate possible errors in these findings. In the article, researchers admitted “it is possible that we were unable to optimize posture and rotation identically on both sides “ as a result of the limited field of view of the imaging equipment.
The device used in the study could only scan a partial foot in a scan. Test subjects had to stand on one foot, then twist and then switch and twist again. Researchers were unable to measure the force with which the subjects moved on each side.
The pedCAT’s field of view accommodates bilateral imaging, which would have allowed researchers to survey both weight bearing feet at the same time, providing helpful insights. The research indicates the importance of weight bearing measurements of a person’s right and left ankle to determine their normal range of motion.
Being able to accurately assess their syndesmosis on one side will help physicians more accurately assess and repair damages to the other.
CurveBeam’s pedCAT technology is the ideal imaging solution because it allows physicians to scan and survey ankles side-by-side for increased accuracy and ease.
CurveBeam and its technical solutions have the potential to revolutionize orthopaedic and podiatric research and care. Visit us at curvebeam.com to learn how pedCAT and other CurveBeam technologies can make a difference in your practice!